Translational Anesthesiology
Worldwide, more than 17% of patients undergoing non-cardiac surgery experience relevant perioperative complications. These complications are associated with increased morbidity and mortality (Pearse et al., BJA 2016) and are particularly common in high-risk patients. Different complications such as wound infections, coagulation disorders, organ dysfunction or cardiovascular events are associated with an inflammatory response and have common immunological and cell biological causes.
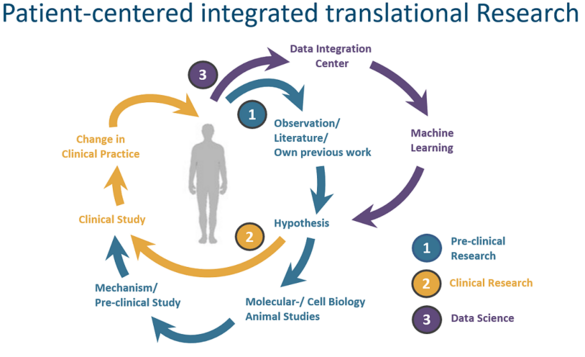
In a young, interdisciplinary team, together with multinational cooperation partners, we are investigating the so far poorly understood inflammatory mechanisms underlying these diseases. Our goal is to reduce the individual burden of perioperative complications for our patients. Using molecular and cell biological methods as well as sophisticated animal models, we develop and test possibilities for prophylaxis and therapy of perioperative cardiovascular events. In clinical trials, we are testing strategies to identify patients at risk and approaches to prophylaxis and therapy of perioperative complications.
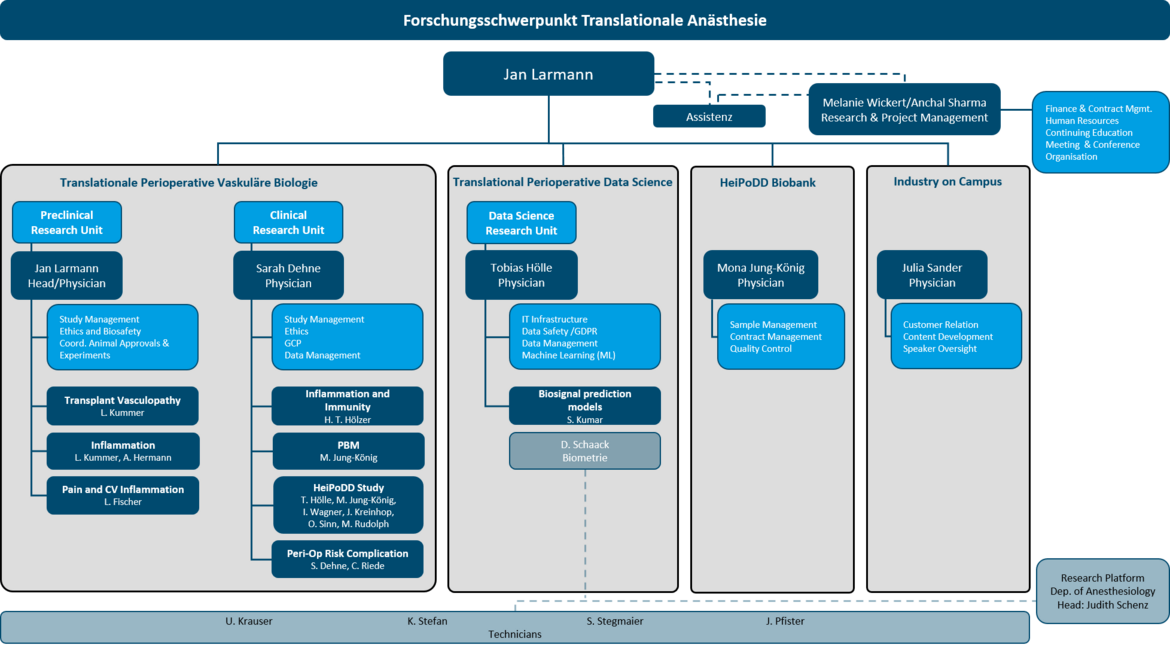
Translational Anesthesiology Reaserch Groups
a. Translational Perioperativ Vascular Biology
b. Translational Perioperativ Data Science
Translational Perioperative Data Science: In order to be able to assess and take into account a patient's individual risk of complications as accurately as possible even before surgery, scientists at Heidelberg University Hospital want to use "machine learning" methods. As part of the "Cognitive Medical Assistant (KoMed)" project, an interdisciplinary team from the Departments of Anesthesiology and General, Visceral and Transplant Surgery will train an algorithm over the next two years to evaluate a large amount of clinical data from patients using Big Data analyses. The aim is to recognize patterns in the data and identify correlations that can be used to create individual risk profiles. KoMed, which was developed jointly with industrial partners, is intended to provide well-founded decision-making support in the future in order to avoid complications through appropriate treatment and care.
Machine learning (ML) algorithms have been increasingly used in the medical field in recent years. Ongoing technical advances in memory capacity and computer power offer the possibility of using ML in the perioperative setting. The literature has demonstrated superiority of ML algorithms over conventional models for predicting perioperative complications. In the HeiPoDD project, patient data are prospectively collected with the goal of developing new models for perioperative risk identification and prediction through this dataset and "explainable artificial intelligence".
BioBank
Heidelberg Perioperative Deep Data Registry and Biomaterial Biobank - HeiPoDD Comprehensive and complete data sets are essential for scientific work in the context of perioperative patient care. For this purpose, the Heidelberg Registry Data and Biobank was established to ensure effective collection and storage of biobank samples and perioperative patient data in a comprehensive database. Biomaterial samples and routine data from patients undergoing major surgical procedures are included in the database after prior consent.
Up to 92 samples (including plasma/RNA/DNA/urine) from nearly 650 patients are stored here, resulting in approximately 51,500 samples currently in the biobank. These samples are combined with an extensive database of routine data (laboratory values, cross-sectional imaging, medication, intraoperative data on surgical course and hemodynamics as well as perioperative outcome and complications) via a medical data information center (MeDIC). Patients are followed up for up to 5 years after their inpatient stay, and follow-up data are added to the existing data set so that information beyond the perioperative setting can be included. Among other things, this overarching data collection enables projects in the field of machine learning and artificial intelligence, for example, to make perioperative risk assessment and decision support in everyday clinical practice possible.
Head of Research Group
Members of the Research group
Topics
AnCHor study
Outcome after intraoperative change of anesthesiologist - Pilot study on the feasibility and effects of a handover checklist.
In everyday clinical practice, there is regularly a change in the anesthesiologist in charge during anesthesia, with the need for a handover that includes all relevant information regarding the patient and the status of the surgery. Retrospective analyses show that such changes have a negative impact on patient outcome. There are recommendations to perform this handover according to a structured scheme. Whether such a scheme in the sense of a checklist has an influence on patient outcome has not yet been investigated in this setting.
The aim of this study is to collect information on the feasibility and data on effect size and associated measures of dispersion of a confirmatory, prospective, multicenter, before-and-after study that answers the question:Does a standardized checklist for intraoperative anesthesiology patient handoffs reduce the rate of postoperative complications?
(Study type: Prospective, monocentric, before-after observational study).
(Julia Sander; PhD student: Timon Streiter)
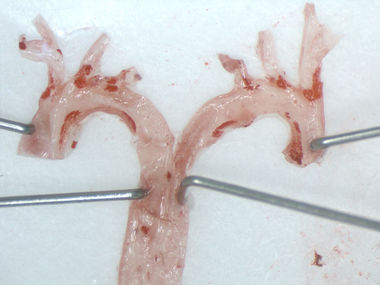
The role of HO-1 in graft vasculopathy.
Heme oxygenase as a therapeutic target in anti-HLA antibody-mediated graft vasculopathy.
In the DFG-funded project "Heme oxygenase as a therapeutic target in anti-HLA antibody-mediated graft vasculopathy", we are investigating the impact of the anti-inflammatory enzyme HO-1 on the development and progression of graft vasculopathy. In various in vitro experiments, we modulate the activity and expression level of HO-1 in endothelial cells to visualize its effects on monocyte adhesion and transmigration in subsequent functional assays. By screening various adhesion molecules at the molecular biology and protein biochemistry levels, we seek to better understand the underlying mechanism. To verify our collected results in vivo, we have established a heterotopic aortic grafting model in mice. Here, a piece of aorta is transplanted between genetically different mouse strains and graft vasculopathy is induced by application of the appropriate antibody. This extremely complex animal model allows us to investigate the protective effect of HO-1 and further therapeutic approaches.
(Laura Kummer)
Importance of regulatory T cells in perioperative stress-mediated destabilization of atherosclerotic plaques.
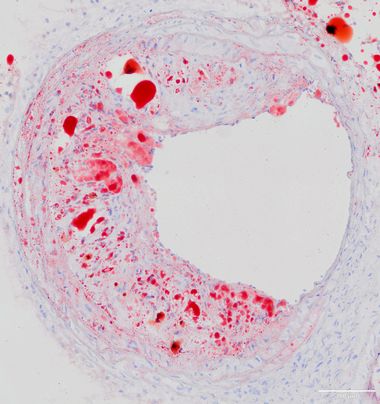
Cardiovascular complications are one of the most common causes of perioperative morbidity and mortality after noncardiac surgery. The underlying mechanisms of perioperative plaque rupture are incompletely understood. However, from previous studies in atherosclerotic mice, immunological processes occurring during surgery condition the progression and destabilization of preexisting atherosclerotic plaques. Furthermore, we observed in a clinical study that preoperative low regulatory T-cell levels correlate with an increased risk of perioperative cardiovascular events.
The aim of this project is to investigate a possible causal relationship of preoperative regulatory T cell levels with perioperatively increasing atherosclerotic plaque vulnerability in a mouse model of perioperative stress, as well as to derive the mechanistic basis using histomorphometric, cell and molecular biology studies.
(Jessica Handke)
KoMed
The Cognitive Medical Assistant (KoMed) - Decision Support by AI on the Highest Data Quality Level.
In the perioperative setting, high volumes of unstructured data are generated on each treatment day. The utilization of such data sources from standard care and their integration with specific research data collected in the course of studies forms the basis for a high-resolution characterization of the perioperative treatment pathway. In the KoMed study, partners at Heidelberg University Hospital (the Department of General, Visceral, and Transplant Surgery, the Institute of Medical Biometry and Informatics, the Department of Medical Information Systems, and the Center for Information and Medical Technology), as well as partners from industry(Mint Medical GmbH, Philips Medizin-Systeme Böblingen GmbH, KARL STORZ SE & Co. KG, and phellow seven GmbH) are preparing such an extensive, detailed data set for further processing in science for the first time. The concerted collection is made possible by the integrated IT environment of the new building of the Surgical Clinic at Heidelberg University Hospital. The emerging pipeline for the multimodal data sources will provide the basis for work with machine learning methods at the Department of Anesthesiology. The goal of the project is to develop clinical discrimination support in the form of an algorithmic tool for risk stratification and prediction of postoperative complications.
(Project leader Jan Larmann, M.D., Ph.D., Deputy project leader Prof. Pascal Probst, M.D.)
(Researchers: Christian Niklas, M.D., Sachin Kumar, Laura Kummer, Balavivek Sivanantham).
Association of perioperative prothrombin complex concentrate and fibrinogen administration and thrombotic complications in patients after liver transplantation.
Liver transplantation is often the only curative treatment option for end-stage liver disease. In view of the scarcity of organs and the increased morbidity and mortality for the patient associated with retransplantation, the avoidance of complications in the course of (liver) transplantation is of particular importance.
An extremely feared complication is thrombosis of the hepatic artery, portal vein and vena cava. A number of risk factors have been identified and described in the literature. However, it has not yet been investigated whether the substitution of certain clotting factors (prothrombin complex concentrate, or PPSB, and fibrinogen concentrate) in the perioperative period plays a role in the development of thrombosis of the hepatic artery, portal vein, or inferior vena cava. Substitution of these blood products is often necessitated by impaired synthesis function due to underlying liver disease.
This is being investigated in a monocentric, retrospective study to further analyze the possible, above-mentioned, relationship and thus contribute to a better understanding of perioperative thrombotic complications in liver transplantation.
(Dr. med. Sarah Dehne; PhD student: Carlo Riede)
Association of perioperative inspiratory oxygen concentration and tumor-free survival after elective oncologic surgery.
An elevated inspiratory oxygen concentration (FiO2) is commonly used in anesthesia, critical care, and emergency medicine. During general anesthesia, the patient is ventilated with a FiO2 between 30% and 100%, depending on the patient's need, the type of surgical procedure, and the anesthesiologist's preference. In this study, we investigate whether a high FiO2 during elective oncologic surgery influences the further course of disease in tumor patients. 1084 patients with colorectal, pancreatic, and hepatocellular carcinoma who underwent surgery at the Department of Surgery at Heidelberg University Hospital between 01/2009 and 12/2016 were included in the study. The primary endpoint is tumor-free survival during the observation period from index surgery to the longest available follow-up. We calculated the mean FiO2 value during surgery for each patient and analyzed data on further disease progression. Patients are divided into two groups according to their FiO2 values and compared in terms of tumor-free survival using Kaplan-Meier analysis.
(Sarah Dehne, MD; PhD student: Verena Spang)
POPART-CVO Study
Association of perioperative aspirin resistance and cardiovascular outcome.
Up to 8 to 13% of non-cardiac surgery patients suffer perioperative cardiovascular complications, some of them severe, such as myocardial infarction, arrhythmias or pulmonary embolism, which account for more than two-thirds of perioperative mortality.
Various studies have already shown the reappearance of perioperatively increased platelet function under aspirin therapy (aspirin resistance). Whether this observation is related to above mentioned cardiovascular events is unclear so far.
In this prospective clinical observational study, vascular surgery patients will now be used to investigate whether the occurrence of perioperative aspirin resistance is associated with the occurrence of small myocardial injury (myocardial injury after non-cardiac surgery, or MINS) and therefore also with increased 30-day mortality. In addition, we will test whether newly developed aspirin resistance can be reversed by in vitro addition of aspirin.
This project is funded by the B. Braun Foundation.
(Dr. med. Sarah Dehne; PhD student: Christian Heck)
Project Sponsor Duration Project leader Funding amount | The Cognitive Medical Assistant (KoMed) - Decision Support by AI on Highest Data Quality Ministry of Science, Research and the Arts Baden-Württemberg March 2020 - February 2022 Dr. Jan Larmann, Ph.D. 2,049,740.00 EUR |
Project Sponsor Duration Project leader Grant amount | Heme oxygenase-1 as a therapeutic target in anti-HLA antibody-triggered transplant vasculopathy DFG grant LA 2343/7-1 2015 - 2020 Dr. Jan Larmann, Ph.D. 215,564.00 EUR |
Project Sponsor Duration Project leader Grant amount | Short-term opioid-mediated effects on atherosclerotic lesion stability Frontier Innovation Fund of the German Excellence Initiative II ZUK 49/2 5.2.159 2016 - 2017 Dr. Jan Larmann, Ph.D. 97,795.00 EUR |
Project Sponsor Duration Project leader Funding amount | Association of PeriOPerative Aspirin-ResisTance and CardioVascular Outcome (POPART-CVO) B. Braun Foundation May 2020 - November 2021 Sarah Dehne, MD 20,000.00 EUR |
Project Sponsor Duration Project leader Funding amount | Quantification of Regulatory T Cells in the Blood of High-Risk Patients Prior to Non-Cardiac Surgery for Risk Stratification of Cardiovascular Complications B. Braun Foundation 2017 - 2018 Jessica Handke 28,000.00 EUR |
Project Sponsor Duration Project leader Funding amount | MET: REevaluation for Perioperative cArdIac Risk (MET-REPAIR): a prospective, multi-center cohort study- Presepsin (sCD14-ST) substudy Mitsubishi Chemical Europe GmbH 2018 - 2020 Dr. Jan Larmann, Ph.D. 21,907.26 EUR |
PD Dr. Stephan Immenschuh, Institute for Transfusion Medicine, Hanover Medical School
Prof. Dr. med. Pascal Probst, Clinic for General, Visceral and Transplantation Surgery, Study Center of the German Society for Surgery; Heidelberg University Hospital
Rosa Klotz, M.D., Department of General, Visceral and Transplantation Surgery, Study Center of the German Society for Surgery; Heidelberg University Hospital
Hannes Kenngott, M.D., Department of General, Visceral and Transplant Surgery, Heidelberg University Hospital
Prof. Dr. Markus K. Diener, MBA, Clinic for General and Visceral Surgery, Freiburg University Hospital
Prof. Dr. med. Arianeb Mehrabi, Clinic for General, Visceral and Transplant Surgery, Heidelberg University Hospital
Prof. Martin A. Schneider, Department of General, Visceral and Transplant Surgery, Heidelberg University Hospital
PD Dr. med. Christian Morath, Heidelberg Kidney Center, Heidelberg University Hospital Dr. Anke Tappe-Theodor, Institute of Pharmacology, University of Heidelberg
Prof. Dr. med. Evangelos Giannitsis, Clinic for Cardiology, Angiology, Pneumology, Heidelberg University Hospital
Prof. Dr. med. Dittmar Böckler, Clinic for Vascular Surgery and Endovascular Surgery, Heidelberg University Hospital
Prof. Dr. Dr. h. c. Markus W. Büchler, Clinic for General, Visceral and Transplant Surgery, Heidelberg University Hospital
Gerd Schneider M.Sc., Department of Medical Information Systems, Heidelberg University Hospital
Dr. sc. hum. Oliver Heinze, Department of Medical Information Systems, Heidelberg University Hospital
Peter Rüdiger, Center for Information and Medical Technology, Heidelberg University Hospital,
Manuel Feisst, Dorothea Weber, Anja Sander, Johannes Krisam, Institute of Medical Biometry and Informatics, Heidelberg University Hospital
Marcin Zaradzki, MD, Clinic for Cardiac Surgery, Heidelberg University Hospital
External
PD Dr. med. Giovanna Lurati Buse, Clinic for Anesthesiology, University Hospital Düsseldorf
Dr. Hans-Jörg Gillmann, Clinic for Anesthesiology and Intensive Care Medicine, Hannover Medical School
Luis E. Tollinche, MD, Department of Anesthesiology & Critical Care Medicine, Memorial Sloan Kettering Cancer Center, New York
Maximiliano Mollura and Prof. Riccardo Barbieri, Department of Electronics, Information and Bioengineering, Plitecnico di Milano, Italy, affiliated with the Massachusetts General Hospital, the Massachusetts Institute of Technology and the Wyss Insitute for Biologically Inspired Engineering at Harvard Univeristy, Boston
Dr. Marianna Laviola and Prof. Dr. Jonathan G Hardman, Interdisciplinary Collaboration on Systems Medicine, Department of Anesthesia and Critical Care, Faculty of Medicine & Health Science, University of Nottingham, UK
Dr. L. Christian Napp, Cardiology and Angiology, Hannover Medical School, Germany
Industry Partners
Mitsubishi Chemical Europe GmbH
Mint Medical GmbH
Philips Medical Systems Böblingen GmbH
KARL STORZ SE & Co KG
phellow seven GmbH
PD Dr. Stephan Immenschuh, Institute for Transfusion Medicine, Hanover Medical School
Prof. Dr. med. Pascal Probst, Clinic for General, Visceral and Transplantation Surgery, Study Center of the German Society for Surgery; Heidelberg University Hospital
Rosa Klotz, M.D., Department of General, Visceral and Transplantation Surgery, Study Center of the German Society for Surgery; Heidelberg University Hospital
Hannes Kenngott, M.D., Department of General, Visceral and Transplant Surgery, Heidelberg University Hospital
Prof. Dr. Markus K. Diener, MBA, Clinic for General and Visceral Surgery, Freiburg University Hospital
Prof. Dr. med. Arianeb Mehrabi, Clinic for General, Visceral and Transplant Surgery, Heidelberg University Hospital
Prof. Martin A. Schneider, Department of General, Visceral and Transplant Surgery, Heidelberg University Hospital
PD Dr. med. Christian Morath, Heidelberg Kidney Center, Heidelberg University Hospital Dr. Anke Tappe-Theodor, Institute of Pharmacology, University of Heidelberg
Prof. Dr. med. Evangelos Giannitsis, Clinic for Cardiology, Angiology, Pneumology, Heidelberg University Hospital
Prof. Dr. med. Dittmar Böckler, Clinic for Vascular Surgery and Endovascular Surgery, Heidelberg University Hospital
Prof. Dr. Dr. h. c. Markus W. Büchler, Clinic for General, Visceral and Transplant Surgery, Heidelberg University Hospital
Gerd Schneider M.Sc., Department of Medical Information Systems, Heidelberg University Hospital
Dr. sc. hum. Oliver Heinze, Department of Medical Information Systems, Heidelberg University Hospital
Peter Rüdiger, Center for Information and Medical Technology, Heidelberg University Hospital,
Manuel Feisst, Dorothea Weber, Anja Sander, Johannes Krisam, Institute of Medical Biometry and Informatics, Heidelberg University Hospital
Marcin Zaradzki, MD, Clinic for Cardiac Surgery, Heidelberg University Hospital
External
PD Dr. med. Giovanna Lurati Buse, Clinic for Anesthesiology, University Hospital Düsseldorf
Dr. Hans-Jörg Gillmann, Clinic for Anesthesiology and Intensive Care Medicine, Hannover Medical School
Luis E. Tollinche, MD, Department of Anesthesiology & Critical Care Medicine, Memorial Sloan Kettering Cancer Center, New York
Maximiliano Mollura and Prof. Riccardo Barbieri, Department of Electronics, Information and Bioengineering, Plitecnico di Milano, Italy, affiliated with the Massachusetts General Hospital, the Massachusetts Institute of Technology and the Wyss Insitute for Biologically Inspired Engineering at Harvard Univeristy, Boston
Dr. Marianna Laviola and Prof. Dr. Jonathan G Hardman, Interdisciplinary Collaboration on Systems Medicine, Department of Anesthesia and Critical Care, Faculty of Medicine & Health Science, University of Nottingham, UK
Dr. L. Christian Napp, Cardiology and Angiology, Hannover Medical School, Germany
Industry Partners
Mitsubishi Chemical Europe GmbH
Mint Medical GmbH
Philips Medical Systems Böblingen GmbH
KARL STORZ SE & Co KG
phellow seven GmbH