PREDICTION OF STROKE OUTCOME AND COMPLICATIONS
OVERVIEW
To decide whether a patient might benefit from a treatment can be very easy in one patient and quite challenging in the next patient. However, in everyday clinical practice we are often faced with difficult decisions which sometimes have to be made immediately. Our group aims to provide evidence that can guide clinicians in making a prognosis on patient outcome and thereby estimate the benefit-risk ratio for a certain treatment. After the acute treatment in stroke, many patients suffer from complications such as recurrent stroke, epileptic seizure, depression or pain. As these complications pose a major burden for stroke patients, our group also focusses on how to predict and treat stroke complications. We are dedicated to the following projects:
- Gut Microbioma and Ischemic Stroke
- Off-label Thrombolysis and Thrombectomy
- Cardiorespiratory Goals in Mechanically Ventilated Stroke Patients
- Multimodal MRI in Ischemic Stroke
Team
Wiss. Mitarbeiter/-innen
Collaborating Scientists
Prof. Dr. Kim Mouridsen, Aarhus, Denmark
Prof. Dr. Leif Østergaard, Aarhus, Denmark
Dr. Arne Potreck, Department of Neuroradiology
Gut Microbiome and Ischemic Stroke (Dr. C. Schneider)
The fact that the mass of an individual’s gut microbiome is twice as heavy as the average human brain and is made up of more cells than there are human cells in a human being emphasizes how important a more detailed exploration of the gut microbiome is. Studies showed that the microbiome is changing after a stroke and that changes in the microbiome are associated with atherosclerosis and cardiovascular disease. Dr. Christine Schneider aims at understanding how the gut microbiome can influence ischemic stroke. As analyzing the microbiome itself can be quite challenging, it might be useful to use biomarkers to describe the microbiome function. Dr. Schneider focusses on one of these biomarkers, Trimethylamine-N-oxide (TMAO), and its role in stroke patients.
Off-label Thrombolysis and Thrombectomy (Anne Tillmann, in cooperation with Prof. Dr. S. Nagel)
The initial trials that led to the approval of alteplase for the treatment of acute ischemic stroke had very strict inclusion criteria, due to the fear of causing symptomatic intracerebral hemorrhage (SICH). The risk of treating patients with off-label criteria with alteplase has not been studied regarding several off-label criteria in a large population. We therefore set out to analyze the large prospective SITS database. 56258 patients who were treated with alteplase were included. 30% of these patients (16740) received off-label thrombolysis. We found that high blood pressure, very severe stroke, previous stroke and diabetes, age and high glucose levels were independent negative predictors and minor stroke was an independent positive predictor of SICH [Mundiyanapurath S et al., EJoN 2018]. Another challenge is the treatment of patients treated with anticoagulants. We studied the effect of a combined approach of intravenous thrombolysis and mechanical thrombectomy in patients that had an elevated international normalized ratio (INR). These patients were not under an increased risk for symptomatic intracranial hemorrhage if patients were treated by mechanical thrombectomy alone if they had an INR > 1.7 and by intravenous thrombolysis and mechanical thrombectomy if they had an INR of 1.2-1.7 [Mundiyanapurath S et al., JNIS 2017].
Cardiorespiratory goals in mechanically ventilated stroke patients (Dr. Tilman Reiff and Oliver Barthel)
Stroke patients with severe clinical symptoms sometimes have to be intubated. This is true for some patients with ischemic stroke and large vessel occlusion undergoing mechanical thrombectomy and patients with large intracerebral hemorrhage or subarachnoid hemorrhage. The ideal cardiorespiratory goals in these patients remain unclear. We studied patients with large vessel occlusion undergoing mechanical thrombectomy in two phases. In the pre-protocol phase, significant hypocapnia, a significant decrease of SBP after intervention and an increase after extubation were observed. After implementing a protocol with theoretically derived target ranges for the end-tidal CO2 (Petco2) and the systolic blood pressure (SBP), severe hypocapnia and hypotension were significantly reduced. Moreover, we found that longer duration of PetCO2 values between 40 and 45 mmHg and higher cumulative dose of norepinephrine were associated with unfavorable outcome [Mundiyanapurath S et al., JNIS 2016]. In a subsequent prospective study, we aimed at analyzing the difference of cardiorespiratory parameters in patients treated under general anesthesia and conscious sedation as a pilot study before starting the SIESTA trial which was led by Dr. S. Schönenberger and Prof. Dr. J. Bösel [Mundiyanapurath S et al. JSCVD 2015; Schönenberger S et al., JAMA 2016]. We found patients treated under general anesthesia were treated with more norepinephrine, had lower blood pressure and higher PetCO values compared to patients treated under conscious sedation. A current study is examining the respiratory parameters in patients with subarachnoid hemorrhage. Further details on this study will be presented shortly.
Multimodal MRI in ischemic stroke (Dr. A. Potreck, Sarah Loebel in collaboration with Prof. Dr. L. Østergaard and Prof. Dr. K. Mouridsen, Aarhus, Denmark)
Predicting outcome in patients with acute ischemic stroke is crucial to decide whether a patient might benefit from therapy. MRI is often used to estimate the infarcted tissue in diffusion-weighted imaging (DWI) and the hypoperfused region in perfusion weighted imaging (PWI). PWI however has some limitations, e.g. in patients with carotid artery stenosis. We compared several perfusion parameters in patients with relevant unilateral symptomatic internal carotid artery (ICA) stenosis. Visually assessed volume of increased time to peak (TTP) did not predict outcome. The time to the maximum of the residue curve (Tmax) however, was an independent predictor in multivariable analysis [Mundiyanapurath S et al., BMC 2016].
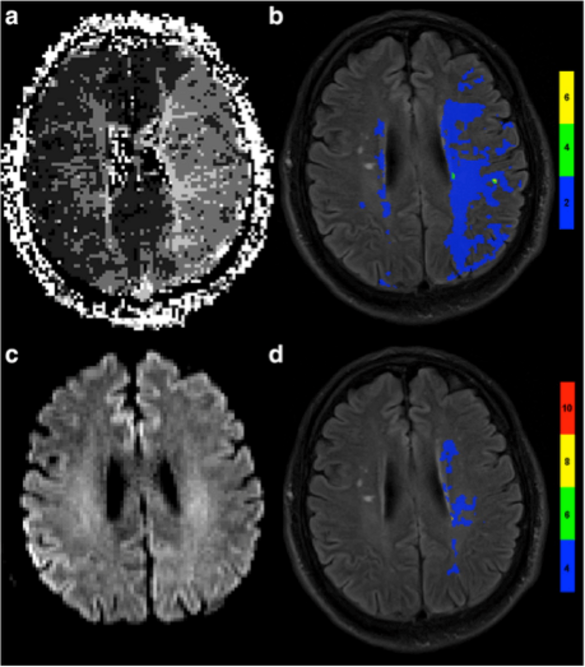
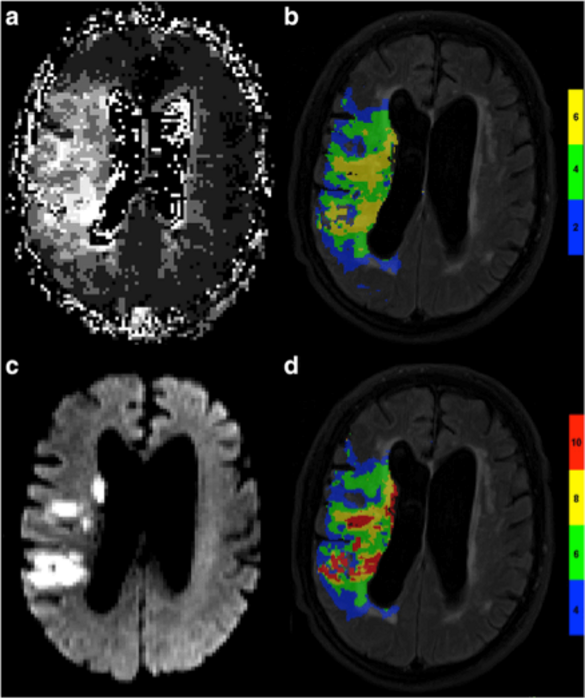
In an even more complicated perfusion profile, PWI with traditional perfusion parameters is difficult to interpret due to uncertainty of the clinical relevance of hypoperfusion. We aimed at finding the optimal perfusion parameters in patients with bilateral high grade ICA stenosis. We found that a new imaging parameter, capillary transit time heterogeneity (CTH) differentiated best between patients with favorable and unfavorable outcome [Mundiyanapurath S et al., PONE 2016]. In another trial, we are aiming at understanding the predictive capacity of CTH in patients with acute ischemic stroke and large vessel occlusion. We found that mildly elevated CTH was associated with favorable outcome. Moreover, patients with higher volume of mildly elevated CTH had lower rates of symptomatic intracerebral hemorrhage. CTH seems to be a marker of microvascular changes that are not seen in traditional perfusion imaging [Potreck A et al., Eur Radiol 2019].
We also studied susceptibility weighted imaging (SWI) as an alternative to assess perfusion, when PWI is not feasible, e.g. allergy against contrast agent. We found that SWI is a predictor of outcome in patients with unilateral ICA stenosis and basilar artery occlusion [Mundiyanapurath S et al., EJR 2016; Mundiyanapurath S et al., PONE 2015].
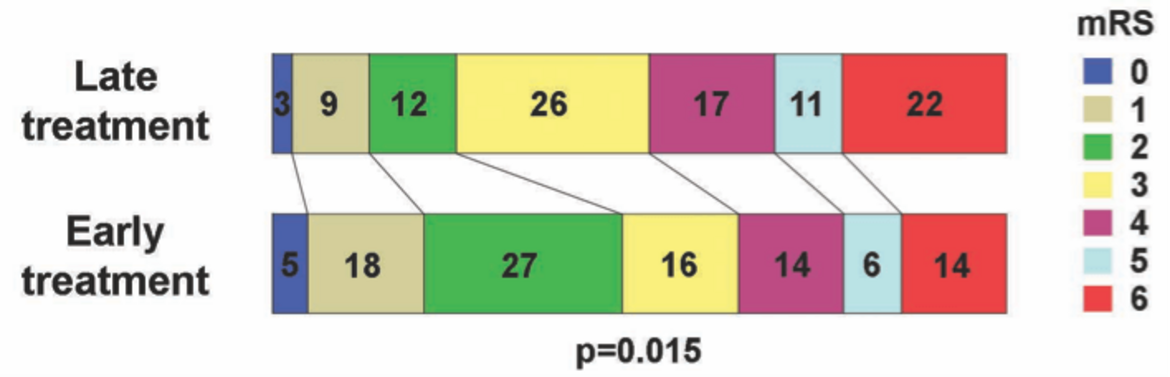
Interestingly, we could also show that outcome in patients with acute ischemic stroke, large vessel occlusion and a significant PWI-DWI mismatch is time-dependent, despite the mismatch. Patients treated in a late time-window had a significantly lower rate of favorable outcome than patients who were treated in an early time-window [Mundiyanapurath S et al. EJR 2017]. These results were confirmed in the DAWN and EXTEND-IA trial.